Did you know around 1 in 8 men in the U.S. will get prostate cancer? It’s key to know about treatments like radiation therapy. This method targets cancer cells and tries to protect healthy tissues. We will cover how radiation therapy works, when it’s used, and what patients should expect.
Radiation therapy is often chosen for early-stage prostate cancer. It’s also used with hormone therapy for advanced cancer. The treatment involves many sessions and close watch. This guide aims to offer deep insights into radiation therapy for making better health choices.
Key Takeaways
- Radiation therapy is crucial for treating prostate cancer, especially for localized cancer.
- External and internal radiation methods aim at cancer cells while saving normal tissue.
- Patients may feel tired or have urinary changes during treatment, but these usually improve.
- Eating well is important during radiation therapy for better recovery and health.
- Monitoring during treatments helps in precise therapy and ensuring patient safety.
- Post-treatment follow-up, like PSA tests, is key for checking recovery.
Understanding Radiation Therapy
Radiation therapy is key in treating cancer, like prostate cancer. It uses high-energy rays to target cancer cells. Cancer treatment aims to destroy these cells by harming their DNA. Knowing how it works helps patients choose their treatment.
At places like Johns Hopkins, over 30 radiation oncologists team up. They create cancer treatment plans together. Radiation therapists, with two to four years of training, make sure treatments are safe.
To protect healthy tissue, doctors use advanced methods. External beam radiation therapy (EBRT) targets only the tumor. Or, brachytherapy places radiation right inside or near the tumor for focused treatment.
A successful plan requires help from dosimetrists and medical physicists, too. They design treatments based on each cancer’s unique traits. Their work ensures equipment and treatments are both safe and effective.
Clinical trials are ongoing at top centers like Johns Hopkins. About half of all cancer patients might need radiation therapy. Understanding its role can make the treatment process smoother for patients.
Radiation Oncology and Prostate Cancer
Radiation oncology is key in treating prostate cancer. It uses radiation therapy as an effective method for different stages. This therapy can be used instead of surgery, especially for localized prostate cancer. It offers outcomes similar to surgery, giving patients multiple treatment options.
There are two main types of radiation therapy in prostate cancer care: external beam and brachytherapy. Advances in external beam technology allow for precise cancer targeting, protecting healthy tissue. Brachytherapy, where radioactive seeds are placed in the prostate, is great for patients with low to intermediate-risk disease.
Treatment planning should be personalized. Prostate cancer can vary, with some tumors spreading quickly and others not. Radiation therapy can help patients with high-risk cancer or as a supplementary treatment, raising cure chances. It also helps those with metastatic disease by slowing its spread and easing symptoms. Patients need to talk about these treatment options with their doctors to choose the right path.

When is Radiation Therapy Recommended?
Radiation therapy is key in treating prostate cancer. Knowing when it’s suggested can greatly impact results. For those with early-stage prostate cancer, radiation therapy is often a cure. It targets tumors well, leading to better survival chances.
When cancer comes back after surgery, radiation therapy becomes crucial. It’s important for patients who didn’t get all the cancer out the first time. Treatment guidelines stress the need to look at the disease’s return and the patient’s health.
Advanced prostate cancer stages also need radiation therapy. It’s used to control symptoms and provide comfort care when the cancer spreads. This method eases pain and other issues from the disease spreading, improving life quality.
Deciding on radiation therapy involves looking at tumor size, grade, and patient age. Doctors follow treatment guidelines to create personalized plans that aim for the best results. For patients dealing with prostate cancer, knowing about these options is essential for recovery.
Types of Radiation Therapy and Their Effectiveness
It’s important to know the radiation therapy types for prostate cancer. Various radiation treatment methods focus on cancer while saving healthy tissue. Options include external beam radiation therapy (EBRT), brachytherapy, and targeted radionuclide therapy.
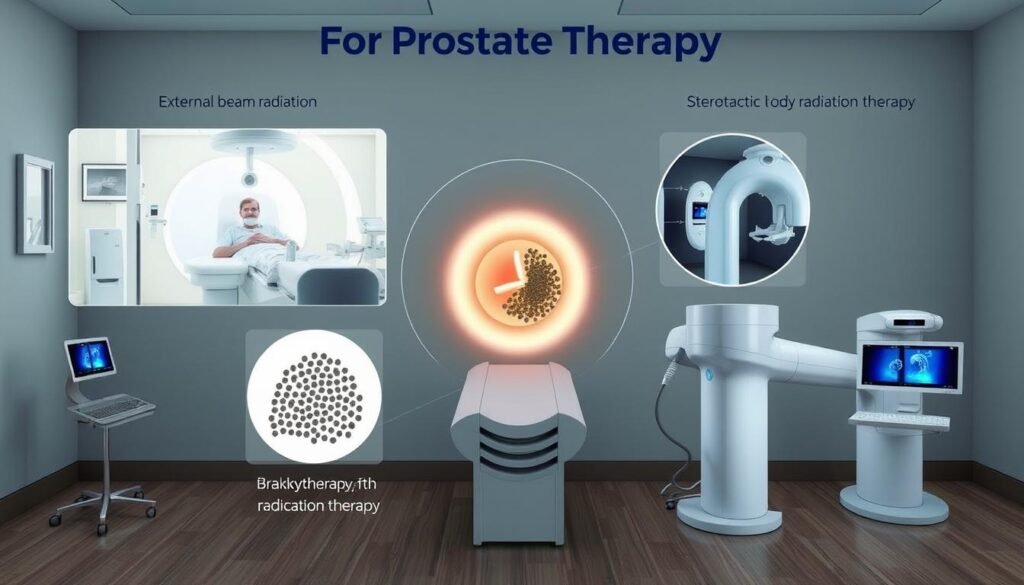
External Beam Radiation Therapy (EBRT) treats many cancer types. It sends high radiation doses to the tumor and protects normal cells. EBRT is given five days a week for a few weeks to work well.
Brachytherapy puts radioactive material close to or in the tumor. It’s often used in prostate cancer and delivers a large dose to the cancer cells. It helps patients a lot because it treats only the needed area.
Targeted Radionuclide Therapy is key for serious prostate cancer or certain neuroendocrine tumors. It treats mainly the cancer cells, aiming to heal while keeping healthy tissues safe.
| Radiation Treatment Method | Common Uses | Effectiveness |
|---|---|---|
| External Beam Radiation Therapy (EBRT) | Various cancers, including prostate | Highly effective for localized tumors |
| Brachytherapy | Head, neck, breast, cervix, and prostate cancers | Effective due to high localized dosing |
| Targeted Radionuclide Therapy | Advanced prostate cancer, gastroenteropancreatic tumors | Focuses on cancer cells, improving therapeutic outcome |
When thinking about treatment effectiveness, it’s good to know radiation therapy’s role. It helps at various cancer care stages as primary or additional therapy. While it works well, it can also cause side effects like tiredness or skin problems.
Learning about these types of radiation therapy lets patients choose their care with doctors. This team effort helps pick the best treatment path.
A Comprehensive Guide to Radiation Therapy
Radiation therapy is key in battling prostate cancer. It uses advanced techniques to target cancer. It also compares well with surgery, helping patients choose wisely.
Overview of Radiation Techniques
The NCCN Radiation Therapy Compendium™ lists several radiation techniques. These are tailored to meet patient needs. Important techniques include:
- 2D/3D conformal external beam radiation therapy (EBRT)
- Intensity-modulated radiation therapy (IMRT)
- Stereotactic radiosurgery (SRS)
Each method targets cancer cells while protecting healthy tissues. Choosing a technique depends on the cancer’s stage and type.
Benefits of Radiation Therapy
Radiation therapy has many advantages. It effectively destroys cancer cells, improving many patients’ outlook. Its wide use underscores its value in cancer care.
- Non-invasive nature, allowing for quicker recovery
- Potential for preserving surrounding healthy tissue
- Convenient treatment schedules, typically five days a week
This makes it a preferred option, especially for treating prostate cancer.
Comparative Analysis: Radiation vs. Surgery
Choosing between radiation and surgery is tough. Each has its pros, cons, and effects to consider. Here are some points to ponder:
| Category | Radiation Therapy | Surgery |
|---|---|---|
| Invasiveness | Non-invasive | Invasive |
| Recovery Time | Faster recovery | Longer recovery |
| Hospital Stay | Outpatient | Possible overnight stay |
| Advantages | Targeted treatment | Immediate removal of tumor |
Talk with a doctor about your cancer and what treatment is best. It will ensure the choice is right for you.

Advanced Techniques in Radiation Therapy
Radiation therapy has improved a lot, making treatments better and more comfortable for patients. There are many advanced techniques for treating prostate cancer. Each one is tailored to meet the specific needs of the patient. The main techniques are External Beam Radiation Therapy (EBRT), brachytherapy, and proton beam therapy.
External Beam Radiation Therapy (EBRT)
EBRT is key for managing prostate cancer. It uses high-energy beams targeted at the tumor. This reduces damage to healthy tissues around it. Innovations like three-dimensional conformal radiation therapy and intensity-modulated radiation therapy have made it more accurate. Studies show that EBRT’s results can be as good as those from radical surgery. It works well for patients with low-risk prostate cancer.
Treatment plans with EBRT can last from one day to eight weeks, depending on what’s needed.
Brachytherapy
Brachytherapy puts radioactive sources close to or inside the tumor. This approach is effective and limits radiation exposure to the nearby healthy tissues. It has become popular for its ability to give a high dose of radiation in a short time. This technique also allows doctors to save the affected organs, meeting the modern standards of care that focus on life quality.
Studies have shown brachytherapy is effective for certain prostate cancer patients. Its outcomes can be similar to those from traditional surgery.
Proton Beam Therapy
Proton beam therapy uses protons, not x-rays, to fight cancer. It targets radiation more precisely, which means less damage to healthy tissues nearby. There’s active research, and many studies suggest promising results for various cancers, including prostate. This technique is becoming more available, adding an important option for treating cancer.
Radiation Therapy Safety and Considerations
Radiation therapy is among the safest treatments today. However, it’s important to manage side effects well for patient health. Careful planning and good side effect management strategies are essential.
Minimizing Side Effects of Radiation
To reduce side effects, many steps are taken. These include:
- Careful radiation planning to pinpoint dosage and area. This limits exposure to healthy tissue.
- Educating patients so they know what to expect. This helps reduce their stress and improves cooperation.
- Using risk assessment to spot potential hazards. Then, making changes to workflows and processes as needed.
While rare, errors in radiotherapy can be serious. Systems like ROSIS and SAFRON offer insights from reported incidents. This helps us learn from past mistakes.
Patient Health and Radiation Safety Measures
Several safety measures protect patients during treatment. They include:
- Following the European Medical Exposure Directive to reduce accidental doses.
- Ensuring professionals are accredited to national standards. This guarantees their expertise in safely delivering treatment.
- Using physical protections, like lead aprons and shields. These protect patients and medical staff from unnecessary exposure.
Regularly reviewing and upgrading safety protocols is crucial. Technologies such as IMRT improve the precision and safety of treatments. This leads to better management of side effects for patients.
| Safety Measure | Description |
|---|---|
| Radiation Planning | Carefully calculate doses and target areas to protect healthy tissues. |
| Patient Education | Inform patients about what to expect, reducing anxiety and ensuring cooperation. |
| Accreditation Standards | Ensure only qualified professionals administer radiation therapy to enhance safety. |
| Physical Shielding | Use of lead aprons and shields to minimize radiation exposure among staff. |
Common Side Effects of Radiation Therapy
Radiation therapy is crucial in treating prostate cancer, but it brings side effects. Knowing the common ones helps patients prepare for and handle changes. These side effects range from stomach problems to tiredness. Handling them carefully is important for a patient’s life quality.
Bowel and Urinary Problems
Patients getting radiation therapy might face stomach and urinary issues. This happens because the prostate is close to these organs. Common side effects include:
- Diarrhea
- Bowel urgency
- Urinating more often
- Pain during urination
- Bladder infections
These problems usually start soon after treatment begins, affecting daily life. It’s important to talk to healthcare providers for help.
Erectile Dysfunction and Other Sexual Issues
Radiation therapy can also affect sexual health. Issues like erectile dysfunction and changes in desire could happen. To manage these effects, options may include:
- Medicine for better erectile function
- Therapy for sexual or relationship issues
- Arginine supplements
Understanding these possible effects is very important. They can affect relationships and how you feel during recovery.
Fatigue and Lymphedema
Fatigue is a common problem with radiation therapy, getting worse over time. Even simple tasks could become harder to do. Sometimes, lymphedema, or swelling, occurs, needing care to relieve symptoms. Talking to doctors about these issues is crucial for proper care.
Understanding these challenges is key for anyone undergoing radiation therapy. Looking for help and getting support from professionals, family, and friends makes the journey easier.
Managing Side Effects During and After Treatment
Understanding how to handle side effects during and after radiation therapy is key to better patient life quality. Patients often deal with symptoms like fatigue and skin changes. Thus, using the right strategies for relief is crucial. Changing diet and having strong support networks are key in this journey.
Diet and Lifestyle Adjustments
Making changes in your diet can greatly help with side effects. Patients might lose their appetite or feel sick, especially with treatments aimed at the abdomen or throat. Eating a well-balanced, nutrient-rich diet can ease these problems. Here’s what can help:
- Eat small meals often to keep energy up.
- Choose high-protein foods to help with healing and keeping weight stable.
- Drink plenty of water to fight off tiredness and nausea.
- Eat bland foods that are easy on the stomach during tough times.
Getting advice from a dietitian can help patients make the right food choices based on their illness and treatment. These dietary changes are a proactive way to handle side effects and boost overall health.
Physical Therapy and Support Networks
Physical therapy is incredibly useful during recovery. Doing exercises meant for your situation can help improve how well you move and relieve tiredness. This is a common issue for those having radiation therapy. Rehab experts can design special plans that build strength and lessen pain.
Support networks are just as crucial. Having family, friends, or support groups around offers emotional support during hard times. They help with practical needs and lend a sympathetic ear, which is vital for dealing with treatment effects. Connecting with people who are going through similar situations creates a strong sense of belonging and understanding.
By changing their diet and keeping strong support networks, patients can better manage side effects during and after treatment.
Conclusion
Radiation therapy plays a key role in treating prostate cancer. It helps both in curing and in easing cancer symptoms. About 50% of cancer patients can benefit from it, improving cure rates every year. It’s crucial for patients to talk openly with doctors to make a good treatment plan.
Radiation therapy is key for early-stage cancers. It can be the main treatment or used with surgery and other therapies. Technology advances, like external beam radiation, help doctors target cancer better and reduce side effects. Keeping up with these advances is vital for choosing the best treatment.
Those facing prostate cancer should see the value in radiation therapy. It’s getting better and more effective with new advances. Working closely with healthcare providers helps patients choose the best treatment. For more on radiation therapy, check out the National Center for Biotechnology Information.