Every year, more than 200,000 men in the United States are diagnosed with prostate cancer. This highlights the value of various treatment options, like radiation therapy. It customizes care for patients, benefiting those with early-stage and advanced prostate cancer.
Knowing when radiation therapy is ideal is crucial for patients on their prostate cancer treatment journey. It works well by itself or with other treatments, such as hormone therapy. It is also a key option for men with cancer that returns after surgery.
Doctors look at cancer stage, risk factors, and what patients want to decide on medical radiation. This guide will look at radiation therapy types and benefits, giving vital details for managing prostate cancer.
Explore more about treatment options to understand how radiation therapy is part of the wider care available for patients.
Key Takeaways
- Radiation therapy can treat both early and advanced stages of prostate cancer.
- It’s effective for recurrent prostate cancer cases, especially after surgical intervention.
- Personalized treatment plans often combine radiation with hormone therapy.
- Modern techniques enhance targeting and minimize side effects.
- Understanding cancer stage and patient preferences are crucial in deciding treatment options.
Understanding Prostate Cancer
Prostate cancer is a serious issue affecting men’s health. It starts in the prostate gland, important for male reproduction. Learning about Prostate Cancer is key. It helps with early spotting and the right treatment.
What Is Prostate Cancer?
It happens when abnormal cells grow in the prostate. Catching it early enhances treatment success. Since it’s often symptom-free at first, screenings are crucial. This is especially true for men over 50 or those with a family history.
Stages of Prostate Cancer
Cancer Staging sorts the cancer by how much it has grown. The stages are:
- Localized Stage: Cancer hasn’t spread outside the prostate. Outlook is usually good.
- Locally Advanced Stage: Cancer has reached nearby areas. This might require tougher treatments.
- Advanced Stage: Cancer has spread further, even to lymph nodes. This stage is more serious.
Knowing the stage helps decide on treatments, like radiation therapy.
Risk Factors Associated With Prostate Cancer
Risk Factors include genetics, lifestyle, and where you live. Important ones are:
- Age: Men over 50 are at higher risk.
- Family History: If prostate cancer runs in the family, risks go up.
- Race: African American men are more likely to get aggressive types.
- Lifestyle Choices: Eating lots of red meat and processed foods can increase the risk.
Knowing these risks helps us be proactive. For those diagnosed, understanding their risks can influence their treatment options. This includes exploring radiation therapy possibilities.
Introduction to Radiation Therapy
Radiation therapy is key in fighting cancer. It uses high-energy rays to break cancer cell DNA. This method focuses on killing cancer cells and saving healthy ones.
Knowing how radiation therapy works helps patients and caregivers. They can then explore the best treatment options for different cancers.
What Is Radiation Therapy?
Radiation therapy is a common cancer treatment. Over half of cancer patients will receive it. It can be done externally or through brachytherapy, where radioactive sources are placed close to the tumor.
These techniques focus energy on specific body parts. They aim for better treatment results with less damage to healthy cells.
How Radiation Therapy Works
Radiotherapy destroys cancer cells with targeted energy rays. Treatment schedules vary, often lasting several weeks. Sessions take 10 to 30 minutes each.
Side effects like hair loss, skin irritation, and fatigue can happen. Managing these effects is vital for the patient’s wellbeing during treatment.
Technology has made radiation therapy more precise. This precision means higher doses to tumors with less risk to healthy tissue. It’s crucial for positive treatment outcomes, for cure or comfort.

| Radiation Therapy Type | Description | Common Uses |
|---|---|---|
| External Beam Radiation Therapy (EBRT) | Delivers targeted energy rays from outside the body | Various cancers, including lung and prostate |
| Brachytherapy | Utilizes radioactive sources placed near or inside the tumor | Head and neck, breast, cervix, prostate |
| Proton Beam Therapy | Employs protons instead of traditional X-rays | Children’s cancers, certain adult tumors |
| Stereotactic Body Radiation Therapy (SBRT) | Delivers high doses of radiation with precision | Small tumors, often in the lungs or liver |
Benefits of Radiation Therapy
Radiation therapy is a key treatment for prostate cancer. It not only reduces tumors but also offers cure in early stages. In more advanced cases, it helps manage symptoms. Targeted radiation allows doctors to attack cancer while keeping healthy tissue safe. This method is crucial in cancer care, helping over 3.5 million people yearly.
How Radiation Therapy Treats Cancer
Radiation therapy fights cancer by breaking the DNA in cancer cells. This stops the cells from growing and dividing. Each treatment is tailored to fit the patient and their cancer type. For example, external beam radiation therapy (EBRT) is used almost every day of the week.
Brachytherapy, another method, puts radiation right into the tumor. Radiation is also known for relieving pain and controlling the tumor. When used with other treatments like chemotherapy, it can improve results. For more information, visit this resource.
Complementary Treatment Options
Adding other therapies to radiation increases its power against cancer. Hormone therapy, for instance, can make tumors smaller and boost survival chances. Chemotherapy also supports radiation in fighting cancer effectively. This multi-angle attack offers patients a better chance at beating cancer. Radiation is adaptable, making it a fundamental part of treating and managing cancer.
When Is Radiation Therapy Recommended for Prostate Cancer?
Radiation therapy is key in treating prostate cancer at various stages. It’s critical to know when it should be used. This knowledge can lead to better patient results. In certain scenarios, its use is effective for treating early-stage, advanced, and recurrent cancers.
Early-Stage Prostate Cancer
Early-stage cancer often sees radiation therapy as a top treatment choice. It’s an option instead of surgery, especially for localized, non-aggressive cancers. Doctors may use genomic tests to see if radiation is the best first step. Thanks to technological progress, short-course radiation can now be done in about five days. This makes treatment easier to follow.
Advanced and Metastatic Prostate Cancer
As cancer moves to advanced levels, radiation therapy helps with symptom relief. It’s key for patients with advanced prostate cancer to improve their life quality. Radiation can ease pain for those who can’t undergo surgery. Adding hormone therapy may slow the cancer, boosting radiation effectiveness. Learn more about hormone therapy options.
Recurrent Prostate Cancer
When cancer comes back, radiation therapy is again a suggested method. An increase in PSA levels might indicate cancer’s return. Radiation targets these areas to help extend life and boost well-being. Keeping up with doctor visits is crucial to adjust treatments when needed.

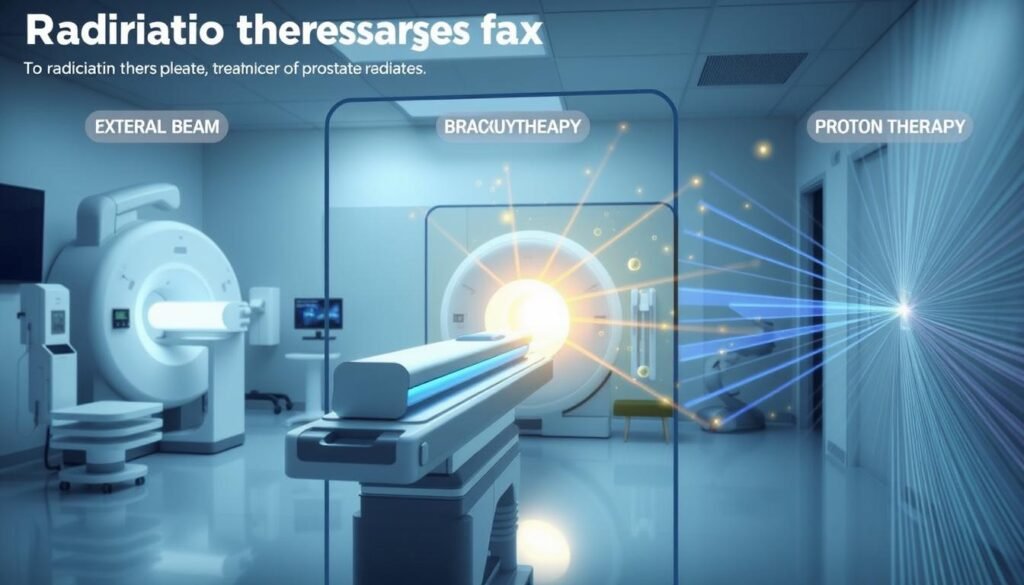
Types of Radiation Treatment for Prostate Cancer
Radiation therapy is key in treating prostate cancer. It has many methods that are designed to help patients. These methods include External Beam Radiation Therapy, Brachytherapy, Proton Therapy, and Stereotactic Body Radiation Therapy. Each method has its unique approach and benefits.
External Beam Radiation Therapy (EBRT)
External Beam Radiation is known for its effectiveness. It often takes a few weeks, with several sessions. High-energy beams are directed at the tumor to kill cancer cells. The most common type used is Intensity-Modulated Radiation Therapy (IMRT).
IMRT targets higher doses at cancer while saving healthy tissue. But, patients might have some side effects. These can include changes in urinating, bowel movements, and sexual function.
Brachytherapy
Brachytherapy is another way to treat prostate cancer. It places radioactive seeds close to the tumor. This can be done using low dose rate (LDR) or high dose rate (HDR) techniques. It targets cancer cells with precision.
Some side effects exist, like urinary incontinence or tenderness. However, new methods like injectable gels help. They reduce the risk to the rectal area from radiation.
Proton Beam Therapy
Proton Therapy is at the forefront of cancer treatment. It delivers radiation in a way that saves healthy tissue. This is especially important in certain prostate cancer cases for precision.
Protons stop at the tumor, reducing damage to healthy areas. Researchers are studying how it compares with other treatments.
Stereotactic Body Radiation Therapy (SBRT)
SBRT is for early-stage prostate cancer. It gives high radiation doses in a short period, usually five days. Advanced technology helps in targeting the cancer accurately.
This approach aims to limit treatment time while being effective. Potential side effects are similar to other radiation therapies. However, the shorter schedule is often easier for patients.
| Type of Radiation | Delivery Method | Typical Duration | Common Side Effects |
|---|---|---|---|
| External Beam Radiation (EBRT) | Multiple sessions with linear accelerator | Several weeks | Urinary changes, bowel issues, erectile dysfunction |
| Brachytherapy | Implants placed near the tumor | Depends on LDR or HDR | Urinary incontinence, tenderness, proctitis |
| Proton Beam Therapy | Targeted proton rays | Varies by plan | Less common side effects due to precise targeting |
| Stereotactic Body Radiation Therapy (SBRT) | Highly focused radiation in few sessions | Five days | Urinary and bowel issues |
Radiation Therapy Recommended: Patient Considerations
Choosing radiation therapy is a vital decision. It affects each person differently. A Radiation Oncologist is needed to create a suitable Treatment Plan. This plan takes into account health issues and personal wishes.
Choosing the Right Treatment Plan
Talking deeply with medical experts is a must to pick the right Treatment Plan. Discussions should focus on:
- Understanding the type of prostate cancer and its stage.
- Evaluating other health conditions that may influence treatment options.
- Considering personal lifestyle preferences and daily routines.
- Reviewing potential side effects and how they may affect quality of life.
- Discussing the duration and frequency of treatment appointments, typically lasting around 15-30 minutes daily, with the actual treatment taking less than 5 minutes.
Consulting with a Radiation Oncologist
Meeting with a skilled Radiation Oncologist is key to understanding treatment complexities. Patients should:
- Ask specific questions regarding the expected outcomes of the proposed plan.
- Inquire about safety measures and protocols in place, particularly concerning radiation exposure to family members.
- Understand the timeline from initial consultation and planning, which may involve a CT scan, to the beginning of the radiation treatment—typically taking 10-14 days.
- Discuss any post-treatment follow-up care, including regular check-ups and monitoring for side effects, which may include skin reactions.
Smart choices about radiation therapy require deep talks and careful thought on all factors. Customized plans improve treatment success and reduce risks and side effects for patients.
Potential Side Effects of Radiation Therapy
Radiation therapy is key for treating cancers like prostate cancer. It has side effects that patients and caregivers should understand. Radiation side effects vary from immediate to long-lasting ones. Knowing about them and managing side effects is crucial. This helps maintain quality of life.
Common Side Effects
Early side effects of radiation therapy can include:
- Fatigue, which may increase during treatment and continue after.
- Skin reactions, like redness, swelling, and dryness, often start in the first two weeks.
- Nausea, especially with radiation near the stomach or abdomen.
- Hair loss in the treatment area, starting around two weeks after beginning treatment.
- Loss of appetite, which can happen early in the treatment.
These side effects are usually mild and treatable. They tend to go away a few weeks after therapy ends. For details on radiation side effects, it’s best to talk to healthcare experts.
Long-Term Effects on Quality of Life
Some late effects can show up months or years after treatment. They depend on factors like the treatment area and radiation dose. Possible late side effects include:
- Bladder and bowel issues, like incontinence or needing to urinate often.
- Sexual dysfunction, affecting things like erectile function or desire.
- An increased chance of getting another cancer in the area that was treated.
- Lasting fatigue that makes daily activities hard.
It’s crucial to know these long-term effects. This way, you can watch your health after treatment and keep good quality of life.
Managing Side Effects
There are many ways to manage side effects from radiation therapy. Some key methods include:
- Using drugs like amifostine to protect against side effects.
- Trying physical therapy or counseling to deal with tiredness.
- Changing your diet to help with loss of appetite or nausea.
- Keeping an eye on your skin health and using lotions as needed.
Talking openly with your doctors can help create a custom plan. This plan can help manage treatment effects better, leading to a better experience for patients.
Research and Advances in Radiation Therapy
The field of radiation therapy is changing fast. This is because of Research in Radiation Therapy and new Technologies. These advances make treatments better and help patients have a better experience. Techniques like MRI-guided radiation therapy and stereotactic body radiation therapy (SBRT) are great examples of this progress.
Latest Techniques and Technologies
Some recent advancements in radiation therapy include:
- 3D Conformal Radiotherapy (3DCRT): It shapes radiation beams to fit the tumor. This reduces harm to nearby tissues.
- Intensity Modulated Radiation Therapy (IMRT): IMRT protects healthy tissues by focusing high doses of radiation on tumor areas.
- Image-Guided Radiotherapy (IGRT): This uses imaging to place treatment more accurately.
- Stereotactic Body Radiation Therapy (SBRT): SBRT uses fewer sessions to deliver high doses of radiation, showing great control of tumors.
Data shows that SBRT controls tumors in about 98% of patients with lung cancer that cannot be operated on. It is also a good non-surgical choice for 85% of patients with hepatobiliary cancer. When used before liver transplants, SBRT reduces the chance of cancer coming back. This leads to better patient outcomes.
Clinical Trials and Ongoing Studies
Clinical trials are crucial to expanding what we know about radiation therapy. These studies look at many types of cancers, like those in the prostate, breast, and lungs. For example, lung cancer patients treated with SBRT now have control rates jumping from 30% to 90%. Their median survival rate is also up to 48 months. These exciting findings highlight the value of joining in Clinical Trials. They greatly help in creating new treatment options.
Conclusion
Radiation therapy is key in treating prostate cancer. It uses different methods, like external beam therapy and brachytherapy. These methods prove to be flexible and successful in treatment.
Patients often enjoy a better quality of life and keep their bodily functions. Choosing the right treatment is essential for people with prostate cancer. Knowing what choices you have is critical. Talking with doctors helps patients learn about their own cases and what they can do.
This is important because radiation therapy has both risks and rewards. A plan made just for you is necessary.
The future of radiation therapy looks bright. Each year, 60 percent of cancer patients in the U.S. get radiation therapy. Thanks to research and new tech, treatment for prostate cancer is getting better.
There’s hope for higher survival rates and better lives. It’s crucial for those affected to make informed choices in their care.