Did you know more than 1 in 8 men will face prostate cancer in their life? This fact highlights the need for effective treatments. Radiation therapy stands out as a key method for tackling prostate cancer. It uses high-energy rays to destroy cancer cells while keeping side effects low. Patients have several radiation therapy options, from external beam radiation to advanced methods like brachytherapy and proton therapy.
This article aims to explain the various radiation therapy types, their functions, and their roles in cancer management. For a deeper understanding, don’t miss exploring the different radiation therapy options detailed online. These methods pave the way for effective cancer treatment.
Key Takeaways
- Radiation therapy is essential for treating prostate cancer. It offers effective care with minimal side effects.
- There are various radiation therapies available, including external beam, brachytherapy, and proton therapy.
- For lower-risk cancers, radiation and surgery offer similar cure rates.
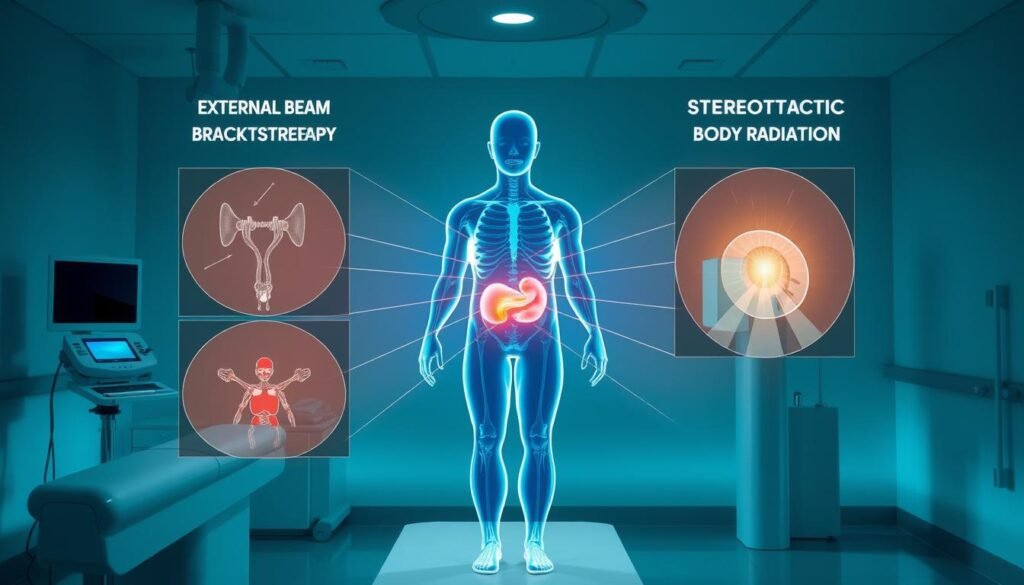
- Techniques like intensity-modulated radiation therapy (IMRT) and stereotactic body radiation therapy (SBRT) improve precision.
- Customized treatment plans consider the cancer’s specifics and patient health.
Introduction to Radiation Therapy for Prostate Cancer
Radiation therapy plays a crucial role in treating prostate cancer. It can be used on its own or with surgery and hormone therapy. This makes it a key tool in fighting prostate cancer.
There are many ways to deliver radiation therapy. External Beam Radiation Therapy (EBRT) is the most common. It targets cancer cells closely, protecting healthy tissue as much as possible. Techniques like Intensity-Modulated Radiation Therapy (IMRT) make this even more precise, which helps patients get better.
Proton Beam Therapy is great for protecting nearby organs like the bladder and rectum. This is important for keeping a good quality of life. Another option, Stereotactic Body Radiation Therapy (SBRT), lets patients finish treatment in just five visits. It’s quick but still very effective.
Brachytherapy is another choice, especially for low-risk or certain intermediate-risk cancers. It’s not used as much as external methods now, but it has its advantages based on the cancer’s traits.
Knowing about these treatments helps patients choose the best one. Going to centers with lots of experience and expert oncologists often leads to better outcomes with fewer side effects.
| Type of Radiation Therapy | Key Features | Typical Duration |
|---|---|---|
| External Beam Radiation Therapy (EBRT) | Most common, precise targeting | 35-45 daily treatments |
| Intensity-Modulated Radiation Therapy (IMRT) | Minimizes damage to healthy tissue | Varies |
| Proton Beam Therapy | Reduces exposure to surrounding organs | Varies |
| Stereotactic Body Radiation Therapy (SBRT) | Delivers treatment quickly, high doses | 5 sessions |
| Brachytherapy | Low-dose rate (permanent) and high-dose rate (temporary) | Varies, typically a single session |
What is Radiation Therapy?
Radiation therapy is a medical treatment that uses high-energy rays to kill cancer cells. It focuses on tumors while trying to save healthy tissue around them. Understanding how it works shows us how it targets cancer cells but often leaves normal ones ok.

There are different types of radiation therapy for cancer. They include external beam radiation and internal radiation therapy. External beam radiation targets specific body parts with cancer. Meanwhile, brachytherapy, an internal type, treats cancers like those in the prostate, breast, and cervix.
There’s also systemic radiation therapy. It sends radiation through your blood to reach cancers spreading in the body. Techniques like radioactive iodine therapy treat some thyroid cancers. Also, targeted radionuclide therapy helps with advanced prostate cancer and neuroendocrine tumors.
Using radiation with other treatments, like surgery or chemotherapy, can work better in fighting cancer. But, it’s important to follow safety steps and dose limits to reduce risks from radiation.
Radiation therapy is key in treating many cancers, accounting for over half of all cases. It can be the main treatment or part of a plan to ease symptoms.
When is Radiation Therapy Used for Prostate Cancer?
Understanding when to use radiation therapy is key for those facing prostate cancer. It is vital throughout different prostate cancer stages. In early stages, where the cancer hasn’t spread, it often is the main treatment. Patients may receive external beam radiation over eight to nine weeks. Or they might get brachytherapy, which uses radioactive seeds to fight cancer.
In advanced stages, choosing when to treat is crucial. Radiation therapy can be combined with hormone therapy to manage serious but non-metastasized cancer. After surgery, it’s important to time radiation right to stop cancer from coming back. This is especially true if treatment timing is key and if there’s a high PSA level.
For advanced prostate cancer showing signs of returning after surgery, external beam radiation offers relief. It eases bone pain when cancer spreads. Techniques like moderate hypofractionation shorten the treatment time but still work well.
In short, radiation therapy depends on the cancer stage and patient needs. It’s about getting the timing right, whether it’s to cure localized cancer, prevent its return, or ease advanced symptoms.
Different Types of Radiation Therapy
When it comes to treating prostate cancer, knowing the different types of radiation therapy is key. The most common kinds are external beam radiation therapy (EBRT) and brachytherapy. Each method works in its own way and suits different patient needs.
External Beam Radiation Therapy (EBRT)
EBRT uses high-energy radiation beams aimed from outside the body to target the prostate’s cancer cells. This technique accurately delivers radiation, protecting the nearby healthy tissue. One type of EBRT, intensity-modulated radiation therapy (IMRT), adjusts the radiation level during treatment. This protects surrounding organs better and reduces side effects, making treatment more effective.
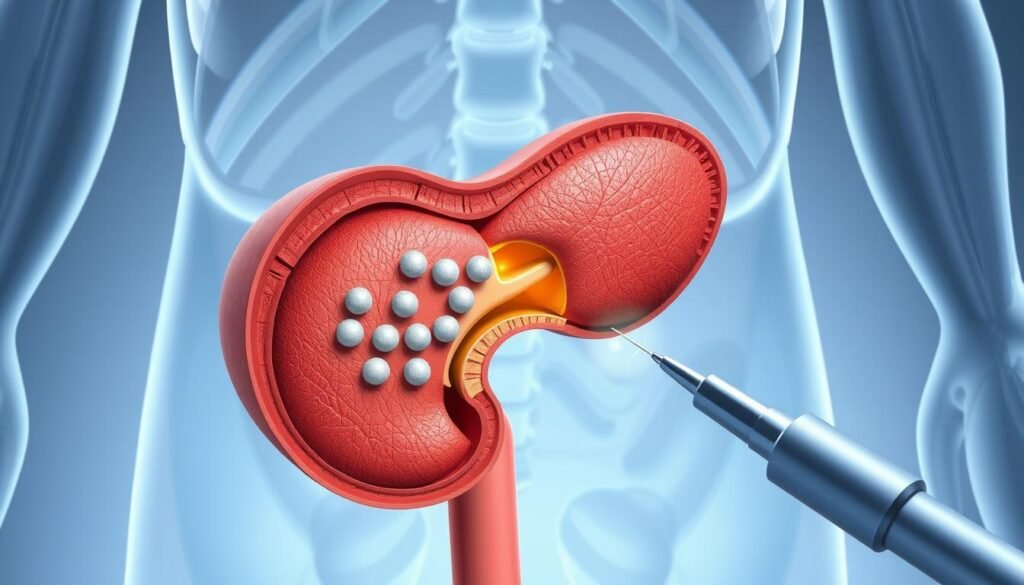
Brachytherapy
In brachytherapy or internal radiation therapy, radioactive seeds are placed inside the prostate. This targets the cancer directly, sparing the surrounding tissues. Brachytherapy works well for cancers that haven’t spread and is quicker than EBRT. Patients should know that this internal treatment has major benefits for certain cases.
External Beam Radiation Therapy in Detail
External beam radiation therapy, or EBRT, is a key treatment for cancer. It uses high-tech methods like 3D-CRT and IMRT. These techniques target the tumor accurately. They also protect the healthy tissue around it.
This makes external radiation a good choice. Knowing about these methods helps patients and caregivers decide on treatments.
Three-Dimensional Conformal Radiation Therapy (3D-CRT)
3D-CRT uses advanced scans like CT, MRI, and PET. They map out the tumor in detail. This lets doctors target it more precisely.
It increases the dose to the tumor while saving the nearby healthy tissue. This results in better treatment outcomes.
- Techniques used: CT, MRI, and PET for precise planning
- Benefits: Higher radiation doses directly to the tumor
- Outcome: Reduced side effects compared to older EBRT techniques
Intensity-Modulated Radiation Therapy (IMRT)
IMRT is a more refined 3D-CRT. It uses adjustable radiation beams. This allows for exact treatment doses.
The beams change strength to focus on the tumor and spare other areas. This method is great for complex tumors.
- Customization: Adjusts beam strength for tailored treatment
- Clinical Application: Effective for complex tumor shapes and locations
- Technology Integration: Often incorporates image-guided radiation therapy (IGRT) for real-time adjustments
EBRT treatment is usually daily, lasting 15 to 30 minutes, over several weeks. This approach is improving all the time.
Research is making it even more effective. And it’s reducing the side effects too.
Brachytherapy Explained
Brachytherapy is a powerful way to fight localized cancers, especially prostate cancer. It involves placing radioactive material right inside or next to the cancer. There are two main types: Low-Dose Rate (LDR) and High-Dose Rate (HDR) brachytherapy, each with its own benefits and treatments tailored to meet different needs of patients.
Low-Dose Rate (LDR) Brachytherapy
LDR brachytherapy uses seed implantation. This means small, radioactive seeds are put in the prostate gland to stay. They give off radiation slowly, from one to seven days. It’s a way to fight the tumor steadily while keeping healthy tissues safe. Impressively, up to 95% of prostate cancer cases treated with LDR brachytherapy are successful.
High-Dose Rate (HDR) Brachytherapy
HDR brachytherapy is different. Here, radiation sources go temporarily into the tumor in short bursts, usually 10 to 20 minutes each time. Depending on the treatment plan, this can happen twice a day for several days or once a week for a few weeks. This technique targets the cancer with high radiation doses quickly. Those choosing HDR may need to stay in the hospital, an important factor to consider.
- Gynecologic cancers (cervical and uterine)
- Breast cancer
- Rectal cancer
- Eye cancer
- Skin cancer
Both LDR and HDR brachytherapy are as effective as the traditional radiation from outside the body. If you’re thinking about this treatment, talk to your doctors for advice on how to prepare and take care after. Following their instructions well is key to safety and the best outcome. For deeper insights, check out brachytherapy procedures provided by reliable medical institutions.
| Brachytherapy Type | Duration of Implantation | Hospital Stay Required | Success Rate |
|---|---|---|---|
| LDR Brachytherapy | Permanently placed (weakens over time) | No overnight stay needed | Up to 95% |
| HDR Brachytherapy | 10-20 minutes per session | May require a hospital stay | Equally effective as LDR |
Advanced Techniques in Radiation Therapy
Advancements in radiation therapy have made cancer treatment better. Specialized techniques now focus on tumors while saving healthy tissue. Proton therapy is especially precise. It sends radiation right to the tumor. This makes it great for treating many cancers.
Proton Beam Radiation Therapy
Proton therapy doesn’t use X-rays. It uses protons. This targets the tumor more and saves normal tissue from damage. It’s now a top choice for treating kids’ cancers and tumors near vital parts. Proton therapy’s improvements have helped patients a lot. They’ve also brought new possibilities in cancer care.
Stereotactic Body Radiation Therapy (SBRT)
SBRT gives large radiation doses in fewer sessions than old methods. It works well for lung, liver, and spine tumors. It’s precise and targets lesions well. SBRT cuts down treatment time and lessens doctor visits. It might also reduce side effects. This makes it a good choice for patients.
Image-Guided Radiation Therapy (IGRT)
IGRT uses real-time images to check the tumor’s location before treating. This makes sure the radiation hits the tumor exactly. It lets doctors adjust the plan as needed. IGRT makes treatments more effective. It also protects healthy tissue better.
These advanced methods are changing cancer care for the better. They offer a care plan tailored to each patient. The way we treat cancer is evolving quickly. For more information on advanced radiation therapy, check out this resource.
Potential Side Effects of Radiation Therapy
Radiation therapy brings several challenges, particularly regarding its side effects. Patients often share various experiences during their treatment. Common early side effects tend to be mild. They are generally manageable. Many get better a few weeks after treatment ends.
As treatment goes on, many report an increase in tiredness. This makes fatigue a significant issue. Skin changes often start in the first weeks of treatment. These changes can cause concern. They may lead to long-lasting effects like skin darkening or scarring. Hair thinning or loss is also common, beginning two to three weeks into treatment.
It’s crucial to manage side effects to improve life quality during radiation therapy. Strategies like using radioprotective drugs, such as amifostine, can help ease discomfort. Patients with radiation to the brain may face headaches, memory issues, and higher risks of secondary tumors over time.
Below is a summary of common radiation therapy side effects:
| Side Effect | Details |
|---|---|
| Fatigue | Commonly experienced; often worsens as treatment continues. |
| Skin Problems | Redness, irritation, and potential scarring in the treated area. |
| Hair Loss | Hair may start thinning two to three weeks after treatment. |
| Nausea and Vomiting | Might occur, particularly if the abdomen is treated. |
| Bowel Issues | Diarrhea and digestive problems can arise, especially with pelvic treatments. |
| Urinary Symptoms | Can include discomfort and infections, particularly in pelvic radiation. |
| Emotional Distress | Some patients experience mental health challenges post-treatment. |
Long-term issues from radiation therapy can include fertility problems and a higher risk of secondary cancers. This highlights the need for strong support during and after treatment. For more on managing these side effects, visit effective strategies.
Choosing the Right Type of Radiation Therapy
When it’s time to choose radiation therapy for prostate cancer, several key factors matter. The cancer’s stage and type heavily shape the treatment method. Early-stage cancers might do well with radiation, but advanced cases often need a different approach.
Considering the patient’s health and personal wishes is also crucial. How well a person can handle treatments depends on their health status. Talking with healthcare professionals helps create a treatment plan that fits the patient’s specific needs. This discussion offers insights into available radiation therapies, like external beam radiation and brachytherapy.
Not all therapies, such as proton therapy, are found everywhere. They’re only at certain cancer centers. But, photon and electron radiation therapies are more common. Knowing the benefits and drawbacks of each helps in making a wise decision. Also, advanced options like stereotactic body radiation therapy (SBRT) focus on the tumor while saving healthy tissue around it.
Having a team of experts from different specialties makes the therapy more effective. This team ensures care that suits the patient’s unique requirements. As treatment goes on, keeping in touch with your medical team is important. It allows for changes to the treatment plan if needed.
Conclusion
Radiation therapy plays a key role in treating prostate cancer. It improves patient outcomes significantly. External Beam Radiation Therapy and Brachytherapy are effective in treatment. They work well for curing cancer and providing relief from symptoms.
Advanced techniques like Intensity-Modulated Radiation Therapy and Stereotactic Body Radiation Therapy are changing the game. They make treatment more precise and lessen side effects. This progress shows how tech improves cancer care.
Education helps patients understand their treatment options. This knowledge encourages them to be more involved in their care. With over 14 million global cancer cases each year, this approach is crucial. About half of all cancer patients could benefit from radiation therapy. This makes it a key part of managing cancer and improving outcomes for prostate cancer patients.
The future of combating prostate cancer looks promising with radiation therapy at its core. The use of advanced technology, thorough treatment plans, and personalized care is vital. By focusing on these areas, patients can explore their treatment options more confidently. They can aim for the best outcomes possible.