Prostate cancer accounted for 23.2% of all male cancer cases in Europe in 2020. This fact shows a critical need for new treatments. MRI-Guided Radiation Therapy (MRgRT) is one such innovation. It combines magnetic resonance imaging with precision radiation therapy. This method allows for real-time treatment adjustments, enhancing tumor targeting accuracy. It has the potential to improve patient outcomes significantly.
Traditional prostate cancer treatments have their limits. MRgRT marks a significant step forward. It uses MRI tech in radiation therapy, changing how we fight prostate cancer. This shift towards MRI-based treatments provides hope. It could lead to better, more patient-focused care in battling prostate cancer.
Key Takeaways
- Prostate cancer is a leading cause of cancer diagnoses among men, necessitating improved treatment modalities.
- MRI-Guided Radiation Therapy offers real-time adjustments to treatment, enhancing targeting precision.
- Innovative treatment options like MRgRT can reduce side effects compared to traditional methods.
- Studies indicate that hypofractionated treatments have promising outcomes for prostate cancer patients.
- MRgRT utilizes advanced imaging to improve accuracy and minimize toxicity during radiation therapy.
- Real-time MRI imaging can help track prostate movement, ensuring effective delivery of treatment doses.
Understanding Prostate Cancer: A Brief Overview
Prostate cancer starts in the prostate gland, an important part of male reproductive health. Its severity can range widely. Thus, knowing about it for early detection and treatment is crucial. In the U.S., it ranks as the second most common cancer in men. About one in eight men will be diagnosed during their life. The prostate cancer overview highlights the value of early discovery and effective treatments.
What is Prostate Cancer?
Prostate cancer involves abnormal cell growth in the prostate gland. It may spread elsewhere. Factors like age, genetics, and environment can increase risk. Specifically, it often impacts men over 65. It’s key for men to talk to doctors about screening methods.
The Impact and Prevalence of Prostate Cancer in the United States
Prostate cancer significantly affects U.S. public health, being a major reason for cancer diagnosis. Yet, most men diagnosed with it do not die from it, thanks to treatment progress. Improved methods, like radiation, are crucial for better results. Studies show over 90% control rate for high-risk cases using radiation and hormone therapy for five years. For those researching effective treatment options, these facts offer hope and guidance in their fight against this illness.
| Statistic | Figure |
|---|---|
| One in eight men diagnosed | Prostate Cancer Incidence |
| Five-year biochemical control rates | Exceed 90% in high-risk cases |
| Grade 3 or higher toxicity rates | Less than 5% |
| No GI toxicities in MR-guided RT | Compared to 14% in CT-guided treatment |
Our knowledge of prostate cancer is constantly growing, highlighting the role of research and clinical trials. With 123 trials for MRI-guided radiation therapy, its benefits for safer, more effective care are clear. Men are encouraged to stay updated on new treatments that reduce side effects and improve success rates.
The Traditional Approaches to Prostate Cancer Treatment
When we look at prostate cancer, old methods mainly used non-invasive external beam radiotherapy. This process sends radiation from outside into the tumor. It aims to hit cancer cells and try to save the healthy ones around it.
Overview of External Beam Radiotherapy (EBRT)
External Beam Radiotherapy stands as the top radiation treatment for prostate cancer. There are modern techniques that make it even better:
- Intensity-Modulated Radiation Therapy (IMRT) allows for precise dose delivery to the tumor.
- Stereotactic Body Radiation Therapy (SBRT) gives large doses in less time.
- Image-Guided Radiation Therapy (IGRT) uses daily images for precise treatment.
- Proton Beam Therapy hits cancer closely, lowering risk to healthy areas.
Studies show radiation therapy and surgery have similar success for low-risk prostate cancer. Patients often have 35 to 45 treatments over 8 to 9 weeks. This makes external beam radiotherapy a strong choice.
Limitations of Conventional Treatment Options
Even with its pluses, External Beam Radiotherapy has downsides. Side effects can include:
- Bowel issues
- Urinary problems
- Erectile dysfunction
- Tiredness
- Lymphedema
Also, the prostate may shift during treatment, causing dose issues and harming healthy tissues. This shows the push for better tech like MRI-guided therapy to boost patient results in traditional treatments.
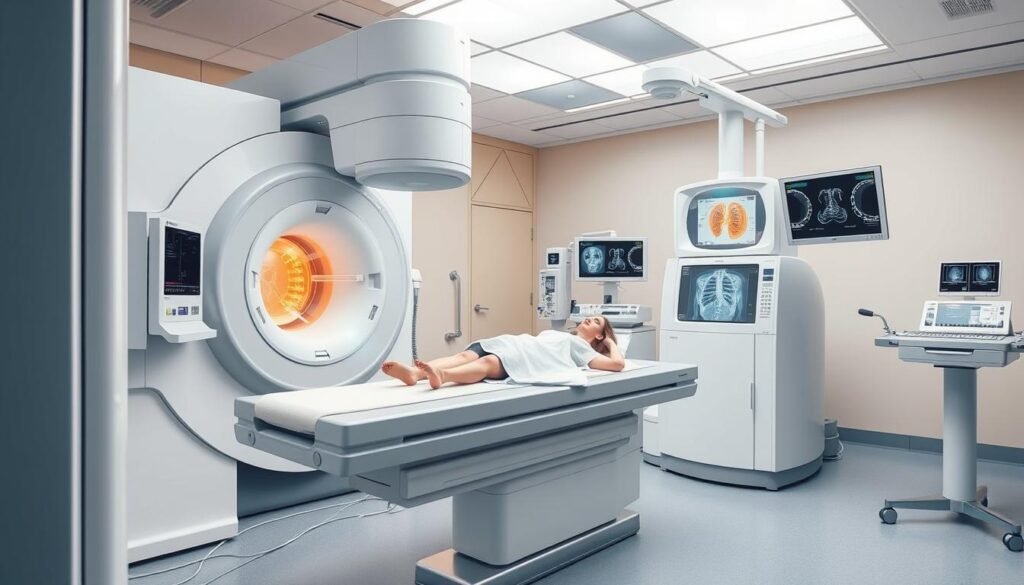
Introducing MRI-Guided Radiation Therapy
MRI-Guided Radiation Therapy is a groundbreaking advance. It combines real-time MRI with precise radiation treatment. This technology greatly improves how tumors and surrounding tissues are seen.
It lets doctors target tumors more accurately during treatment. Being able to see organs in detail helps oncologists plan better. It also helps avoid harm to healthy tissues.
What is MRI-Guided Radiation Therapy?
MRgRT brings MRI into the radiation therapy process. Since 2014, technologies like ViewRay and Elekta have changed cancer care. They make extra imaging sessions unnecessary, making things easier for healthcare workers.
ViewRay now has 45 MRgRT units worldwide. This shows how quickly it’s become a key part of cancer treatment.
The Role of Magnetic Resonance Imaging in Oncology
MRI is very important in cancer care. It gives clear pictures of soft tissues that other methods can’t. This is especially useful for treating certain cancers, like those in the pancreas or abdomen.
In studies, MRgRT has been effective, giving patients better-guided treatment. For more details on these advances, see this source.
How MRI-Guided Radiation Therapy Works
MRI-guided radiation therapy (MRgRT) is changing cancer care. It uses advanced imaging to guide radiation. This method allows doctors to target tumors very precisely. Every treatment plan is made just for the patient. This helps doctors see and adjust to different types of tumors.
Combining Imaging and Radiation Treatment
Imaging and radiation merge smoothly in MRgRT. Doctors can see the tumor move as they treat it. This helps them aim better, protecting healthy tissue nearby. Using the ViewRay MRIdian system, for example, lets treatment adjust on the fly. This makes sure radiation is given out perfectly.
Real-Time Imaging and Tumor Tracking
Real-time imaging is key for tracking tumors in moving parts of the body like lungs. It cuts down mistakes by accounting for patient movement. This method makes radiation fields smaller and more exact. This makes treatment better and might even make visits shorter.
![]()
| Key Features | Description |
|---|---|
| Real-Time Imaging | Monitors tumor position continuously during treatment for precise targeting. |
| Tumor Tracking | Adapts to physiological changes, reducing treatment inaccuracies. |
| Precision Radiation Fields | Delivers focused radiation doses, protecting healthy tissues. |
| Personalized Treatment Plans | Each plan is tailored to the individual patient, enhancing effectiveness. |
These improvements make MRgRT very good for soft tissue tumors. It lets doctors give higher doses safely. This reduces the number of visits. Patients find treatment comfortable and efficient.
Benefits of MRI-Guided Radiation Therapy in Prostate Cancer Treatment
MRI-Guided Radiation Therapy (MRgRT) brings big changes for prostate cancer patients. It improves therapy by pinpointing tumors with high accuracy. This means doctors can avoid harming healthy tissue, making treatment safer. The precision lowers risks of damaging nearby organs unlike old methods.
Enhanced Precision with MRgRT
MRI tech combined with radiation therapy allows doctors to watch tumors closely. They can adjust the treatment daily based on tumor changes. This means every patient gets a plan just for them. Studies show this method controls cancer better by using specific radiation doses.
Reducing Treatment-Related Toxicity
Lowering side effects is key in cancer care. MRgRT makes this possible by fine-tuning radiation doses. Research shows its side effects are fewer than traditional radiation therapy. This leads to less harm to the stomach and urinary areas, improving life during and after treatment.

| Study | Comparison | Outcome |
|---|---|---|
| MRC RT01 | 74 Gy vs. 64 Gy | Superior biochemical control rates |
| RTOG 0126 | 79.2 Gy vs. 70.2 Gy | 70% biochemical control at 7 years |
| CHHiP | 60 Gy in 20 fractions vs. 74 Gy in 37 fractions | Noninferior outcomes in low-risk patients |
| HYPO-RT-PC | 42.7 Gy in 7 fractions | Noninferior to conventional fractionation |
| PACE B | 36.25 Gy in 5 fractions vs. 78 Gy in 39 fractions | Similar toxicity rates |
MRgRT improves prostate cancer treatment in many ways. It makes therapy more effective and patients’ experiences better. It focuses on precise treatment and fewer side effects, pointing towards a bright future in cancer care.
Comparative Advantages Over Traditional Radiation Techniques
In the world of cancer treatment, comparing old and new methods is key. Image-Guided Radiotherapy (IGRT) has improved how precise and accurate treatments can be. Yet, IGRT has its own set of challenges, especially in seeing changes in soft tissue during treatment.
Limitations of Image-Guided Radiotherapy (IGRT)
IGRT has made radiation treatment better but it faces some issues.
- Soft Tissue Visualization: Old techniques might not show soft tissues well, making it hard to target tumors.
- Real-Time Adjustments: IGRT usually uses images taken before treatment, which might miss changes during radiation.
- Motion Considerations: It can be hard to track moving tumors and nearby organs, adding uncertainty during treatment.
How MR-Linac Technology Improves Treatment Outcomes
MR-Linac technology is a big leap forward. It combines Magnetic Resonance Imaging with linear accelerators. This tackles many issues seen in standard IGRT:
- Real-Time Imaging: MR-Linac allows for ongoing visual checks during treatment, enabling quick changes.
- Enhanced Tumor Targeting: It shows soft tissues clearly, making it easier to hit tumors accurately.
- Adaptive Treatment Plans: This technology adjusts treatments based on live data, raising the quality of care.
MR-Linac technology sets new standards in treatment, offering better outcomes for patients. Its pinpoint accuracy and reduced side effects make it a groundbreaking tool in cancer care.
| Aspect | Image-Guided Radiotherapy (IGRT) | MR-Linac Technology |
|---|---|---|
| Soft Tissue Contrast | Limited | Superior |
| Real-Time Imaging | No | Yes |
| Treatment Adjustment | Pre-treatment only | Continuous during treatment |
| Adaptive Planning | No | Yes |
Current Clinical Practices and Technologies in MRgRT
The introduction of MR-Linac systems has changed how we treat prostate cancer. Tools like Elekta Unity and ViewRay MRIdian let doctors adapt radiotherapy every day. This means they can fine-tune treatment for each patient’s unique needs.
Overview of MR-Linac Systems
MR-Linac combines MRI with radiation therapy for better precision. A survey of 52 centers showed that 82.7% are using these systems:
| MR-Linac System Type | Number of Centers (%) |
|---|---|
| 0.35T MR-Linac | 23 (53.5%) |
| 1.5T MR-Linac | 20 (46.5%) |
Around 58% of centers also use MR contrast agents to improve imaging. Gadoxetate is a popular choice for this.
Daily Adaptive Radiotherapy in Clinical Settings
Daily adaptive radiotherapy lets doctors change treatment plans each day. This improves results and lowers side effects. For example, using MR-guided methods reduces certain urinary side effects compared to traditional methods.
The development of MR-Linac systems shows how treatment is getting better. As these practices keep improving, research will find the best ways to use these technologies. For more details on treatment methods, check this resource.
Patient Experiences and Clinical Outcomes
Patient experiences are key to understanding MRI-Guided Radiation Therapy. This treatment focuses on a patient-centric approach. It makes sure patients get the medical care they need and feel respected.
Patient-Centric Treatment Models
A study with 170 patients from five centers showed high satisfaction with their treatment. MR-guided adaptive radiotherapy (MRgART) on the MR-Linac (MRL) had an 84% positive response. This proves that focusing on patients’ needs and comfort works well.
- 90% of patients felt calm during treatment.
- 79% reported that their treatment expectations were met.
- 75% experienced an unexpectedly low level of side effects.
- 86% maintained engagement in social activities throughout therapy.
Success Rates and Side-Effect Profiles
Clinical outcomes show promising treatment success. Of 113 mainly male participants, aged around 69, responses were consistent. A scale was used to measure this, showing a reliability score of 0.8. About 28% felt tingling during treatment, but few felt uncomfortable.
| Aspect | Response Rate |
|---|---|
| Patients who felt calm | 90% |
| Expectations met | 79% |
| Low side effects experienced | 75% |
| Engagement in social activities | 86% |
| Patients feeling discomfort on bed | 8% |
These results highlight the success of MRI-Guided Radiation Therapy. Personalized care is key for people dealing with prostate cancer. It shows that this method can improve patient experiences and clinical results.
Future Directions for MRI-Guided Radiation Therapy
The field of MRI-guided radiation therapy (MRgRT) changes fast, thanks to new technology and clinical research. These improvements lead to better care and new treatment plans. They highlight the future of MRgRT in cancer care.
Emerging Technologies and Techniques
New developments, like the MRIdian® or ViewRay systems, mark big steps forward. They have a 0.35-T MRI and special cobalt radiation sources. This tech makes treatments more precise and tailored.
Clinicians can now see and tweak treatments as they go, responding to how patients are doing in real-time. As more people learn about MRgRT, its use is growing in top medical centers around the world.
The Importance of Ongoing Research and Trials
Research trials are essential for understanding MRgRT’s full potential. For example, a Phase 2 trial for pancreatic cancer with the MRIdian SMART system has shown very good survival rates. These trials help find new ways to fight other hard-to-treat cancers, based on recent successes.
Looking ahead, the future of MRgRT relies on more studies and proof. This is how these pioneering approaches will make cancer treatment better.
| Technology | Key Features | Benefits |
|---|---|---|
| MRIdian® (ViewRay) | 0.35-T MRI, 60Co sources, adaptive RT | High precision, real-time adjustments |
| SMART System | Enhanced imaging, personalized dosing | Improved survival rates, fast treatment delivery |
| Commercial MR-Linacs | Integrated MRI-guidance with RT | Better targeting, safer high-dose delivery |
Challenges and Considerations
Even though MRI-Guided Radiation Therapy (MRgRT) has improved, it still faces significant hurdles. High costs for equipment and the need for special training are big obstacles. These barriers make it tough for clinics to use these advanced tools. To successfully integrate this tech, clinics must invest money and train their staff well in MRI.
Pitfalls of MRgRT Implementation
The accuracy of MRgRT treatment is vital. But, machine-based magnetic fields vary, leading to potential dose distortion. For example, “dose hot spots” can increase by up to 48% at certain body parts, affecting treatment success. High exit skin doses pose another risk, due to magnetic effects on radiation.
This means careful quality assurance (QA) plans are essential. They keep patients safe during treatment.
Understanding Limitations in Current Studies
There are noticeable gaps in the research on MRgRT’s effectiveness. Most studies are small and don’t look at long-term effects well. This makes it hard to know if MRgRT is truly beneficial for personalized treatments. Yet, research continues, examining how patient chemistry can alter imaging results.
For MRgRT to succeed in cancer care, balancing tech progress with these issues is crucial. This approach aims to improve care for patients and make MRgRT mainstream in oncology.
Conclusion
MRI-Guided Radiation Therapy is a big step forward in treating prostate cancer. It’s more precise and has fewer side effects than old methods. With over 100 MRI systems worldwide, this blend of live imaging and adaptive planning is changing patient care.
This shift towards MRI in radiation therapy shows great promise for better outcomes. Especially for cancers that are hard to treat.
There’s a lot of work being done on MRCT generation algorithms. This shows how important MRI is in radiation therapy. But, we need strong studies to really see its benefits over traditional methods. If proven, MRI-Guided Radiation Therapy will enhance how we treat cancer and lead to new breakthroughs.
As technology gets better, choosing the right patients for MRI treatments is key. MRI is becoming crucial in planning for prostate cancer treatments and more. To understand the full benefits of MRI in treating prostate cancer, check out this comprehensive summary. The future looks bright for improving treatment methods and patient care.