Did you know about the 1 in 8 men risk of prostate cancer? This fact underscores the importance of understanding prostate cancer stages. The TNM system is a tool developed by the American Joint Committee on Cancer. It uses Tumor size (T), lymph Node involvement (N), and Metastasis (M) to categorize the cancer.
This method plays a key role in gauging the disease’s spread and choosing treatment. It allows for more tailored and effective treatment plans. By understanding tumor size and spread, doctors can improve prostate cancer outcomes for patients. This makes learning about prostate cancer staging crucial for better care decisions.
Key Takeaways
- The TNM staging system is essential for determining the extent and nature of prostate cancer.
- Understanding tumor size and spread directly impacts treatment decisions.
- Staging guides healthcare providers in predicting prostate cancer prognosis.
- The classification of cancer into T, N, and M categories aids in personalized treatment plans.
- Regular assessment of staging can lead to timely adjustments in treatment strategies.
Understanding Prostate Cancer Staging
Prostate cancer staging tells us how much the disease has spread in the body. It helps answer important questions. These include the tumor size and if it has moved to lymph nodes or other places. Knowing the stage is key to planning the best treatment and understanding what to expect.
The AJCC/UICC TNM system breaks prostate cancer into stages 1 through 4. The stage depends on how much the cancer has spread. For example, Stage 1 means the cancer hasn’t spread beyond the prostate. By contrast, Stage 4 means it has reached other parts of the body. This system helps doctors create a treatment plan that suits each patient.
Doctors use exams, imaging, and biopsies to stage the cancer. The Gleason score and PSA levels are also important. They help doctors figure out how likely the cancer is to grow quickly. This way, they can put patients into different risk groups. These are low-risk, intermediate-risk, and high-risk.
Patient and family awareness of prostate cancer stages is crucial. It helps in understanding treatment options and what to expect. For more information on treatments like hormone therapy for prostate cancer, look for reliable sources.
| Prostate Cancer Stage | Description | Five-Year Survival Rate |
|---|---|---|
| Stage 1 | Cancer is confined to the prostate. | 100% |
| Stage 2 | Localized cancer cells within the prostate gland. | 100% |
| Stage 3 | Locally advanced cancer. | 100% |
| Stage 4 | Cancer has spread to lymph nodes or other body parts. | 34% |
What is the TNM Staging System?
The TNM staging system is key for understanding how prostate cancer develops. It looks at tumor size, lymph node involvement, and if cancer has spread far.
Within the TNM system, ‘T’ refers to the size of the main tumor. T0 means there is no tumor. T4 means the cancer has grown into nearby areas like the bladder or rectum. This helps show how far the cancer has spread locally.
‘N’ stands for lymph node involvement. N0 shows no cancer in nearby lymph nodes, and N1 shows cancer is present in these nodes. Knowing about lymph node involvement helps doctors plan treatment.
‘M’ is about whether the cancer has spread to distant areas. M0 means the cancer hasn’t spread far, while M1 means it has. This is crucial for choosing treatments and understanding the cancer’s impact.

Doctors use the TNM staging to give prostate cancer a stage from 0 to IV. Each stage shows how advanced the cancer is. This helps doctors create better treatment plans, aiming for the best possible outcomes.
| Category | Definition |
|---|---|
| T (Tumor) | Describes the extent of the primary tumor, from T0 (no tumor) to T4 (tumor extends into nearby structures). |
| N (Node) | Indicates lymph node involvement, with N0 meaning no spread and N1 indicating involvement of nearby lymph nodes. |
| M (Metastasis) | Determines whether cancer has spread to distant parts of the body (M0 for no spread, M1 for metastasis). |
The Importance of Staging in Prostate Cancer
Staging is key in knowing how to tackle prostate cancer. It helps find the best treatment planning for a patient. Knowing the cancer’s spread helps choose between surgery, radiation, or hormone therapy.
The TNM system gives details on tumor size, lymph node status, and if it’s spread. For example, stage 1 is cancer only in the prostate. Stage 4 means the cancer has spread far and needs stronger treatment.
Many tests help make staging more precise. New technologies and markers offer deeper insights into cancer. This leads to better treatment plans. Paying attention to PSA levels and tumor details helps doctors care better for their patients.
| Staging Number | Description | Implications |
|---|---|---|
| Stage 1 | Cancer confined to the prostate | Generally excellent prognosis with localized treatment |
| Stage 2 | Cancer present in prostate but larger | Potential for surgical and radiation options |
| Stage 3 | Cancer has spread beyond the prostate | Requires aggressive treatment approaches |
| Stage 4 | Cancer has metastasized to other body parts | Systemic therapy and palliative care typically needed |
Staging is very important. It helps doctors decide the best way to increase survival and life quality for patients. These decisions are essential for patients and advances in this area help shape treatments for the future.
For more info on prostate cancer staging, check this link.
Prostate Cancer Staging Explained
Knowing what definition of staging means is key for patients and doctors. It’s about finding out how advanced the cancer is. This step is key because it helps to choose the best treatment. Doctors use exams, scans like CTs and MRIs, and tissue samples to stage cancer. It helps sort prostate cancer into stages, which shapes treatment and care.
Definition of Staging in Cancer Treatment
The prostate cancer staging explained method uses the TNM system. It looks at tumor size, if lymph nodes are involved, and if cancer has spread. Each stage has specific features, like the Gleason score and PSA levels. Stage I cancer might just be watched closely, but Stage IV might need stronger treatments.
How Staging Influences Treatment Decisions
Staging makes a big difference in choosing treatments.
- Stage I: Cancer hasn’t spread much and treatment aims to cure.
- Stage II: More advanced but still focused on curing.
- Stage III: Cancer has grown beyond the prostate, using surgery and radiation together.
- Stage IV: Cancer has spread far, so treatment aims to ease symptoms and extend life.
Each stage changes how doctors treat the cancer and talk to patients about their care.
| Stage | Characteristics | Treatment Approach |
|---|---|---|
| Stage I | Localized, Gleason score 6 or less | Active surveillance or surgery |
| Stage II | Localized but with higher Gleason scores | Surgery or radiation therapy |
| Stage III | Spread outside the prostate, possibly affecting seminal vesicles | Combination of treatment options |
| Stage IV | Metastatic spread | Palliative care, hormone therapy |
In short, staging impacts treatment greatly and helps in making smart choices for prostate cancer care. By carefully checking the tumor’s details, doctors can pick the best therapy, aiming to make patients’ lives better.
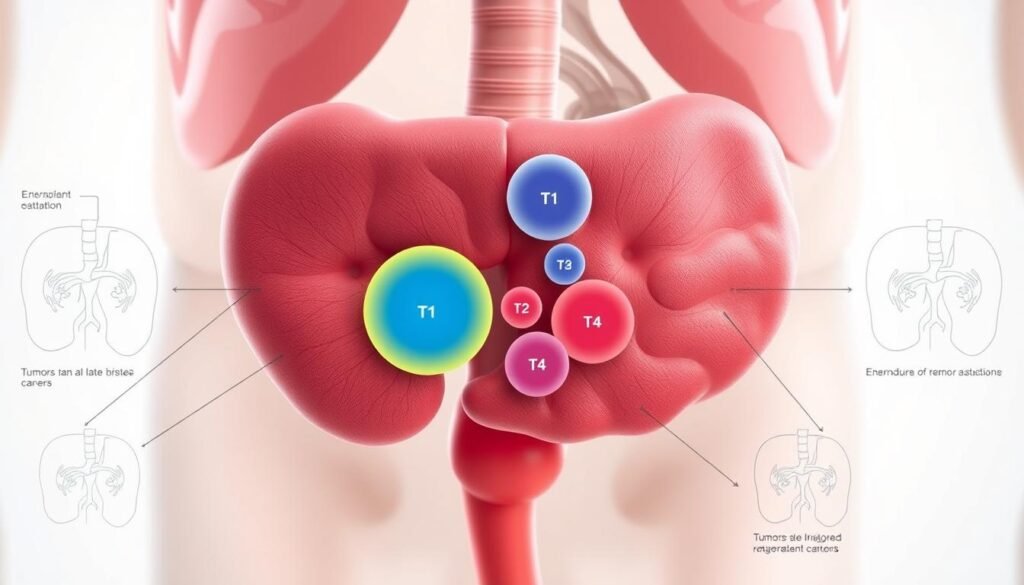
Tumor (T) Classification in the TNM System
The TNM system helps doctors understand tumors in prostate cancer. The T classification looks at the primary tumor’s size and spread. Knowing this is vital to decide how to treat the cancer.
Overview of T Stages: T1 to T4
T stages in the TNM system go from T1 to T4. Each stage tells us about the tumor’s size and spread:
| T Stage | Description |
|---|---|
| T1 | Small tumors that are not detectable through standard examinations. |
| T2 | Cancer that remains confined to the prostate. |
| T3 | Tumor has spread beyond the prostate capsule. |
| T4 | Cancer has invaded adjacent organs or structures. |
Each T stage is crucial for creating a treatment plan and predicting the results. Knowing if cancer is T1, T2, T3, or T4 helps doctors make detailed care plans.
Significance of Each T Stage
Understanding T stages in prostate cancer is very important. For example, T1 means the tumor is small and contained, which is good news. But T4 means the cancer is more aggressive and has spread, which is more serious.
Looking closely at tumor stages helps doctors make good choices for extra treatments. This might include other therapies if there’s a chance cancer has spread to lymph nodes. This way of combining tumor size and lymph node status shows how crucial accurate staging is. It makes patient care better. For more on cancer staging, see this resource.
Lymph Node (N) Classification in Prostate Cancer
Lymph node involvement is key in understanding prostate cancer’s progression. The TNM N staging shows if cancer has reached nearby lymph nodes. It tells us about the spread of the disease. N0 means no lymph nodes are involved, and N1 means cancer is in nearby lymph nodes. This information helps doctors plan the best treatment.
Knowing how far cancer has spread to lymph nodes is crucial for treatment. Studies show that the number of cancerous lymph nodes affects survival rates. For example, patients with one affected lymph node have a 75% to 80% chance of living for five more years. But, if more than five nodes are affected, chances drop to 20% to 30%.
Traditional scans like CT and MRI often miss cancer in lymph nodes. They have a 39% to 42% success rate in finding cancer and an 82% chance of correctly identifying nodes without cancer. This means doctors might miss cancer in small lymph nodes.
New MRI techniques are much better at spotting cancer in lymph nodes. They are good at showing the difference between lymph nodes and nearby blood vessels. This leads to better diagnosis. Studies have shown that these new methods can find small cancers in lymph nodes in 79% to 85% of patients. Before, these patients were mistakenly thought to have no lymph node cancer.
Here’s a list of imaging methods for checking lymph nodes:
- Conventional CT and MRI
- MRI with Ultra-small Super Paramagnetic Iron Oxide (USPIO)
- PET/CT-FDG
- PET/CT-choline
- PET/CT-PSMA
- PET/CT-FDHT
- PET/CT-FACBC
The TNM system is essential for understanding lymph node status. It combines physical exams, PSA tests, and Gleason scores. This helps doctors find the most suitable treatments. It also ensures patients are closely watched as their condition changes.
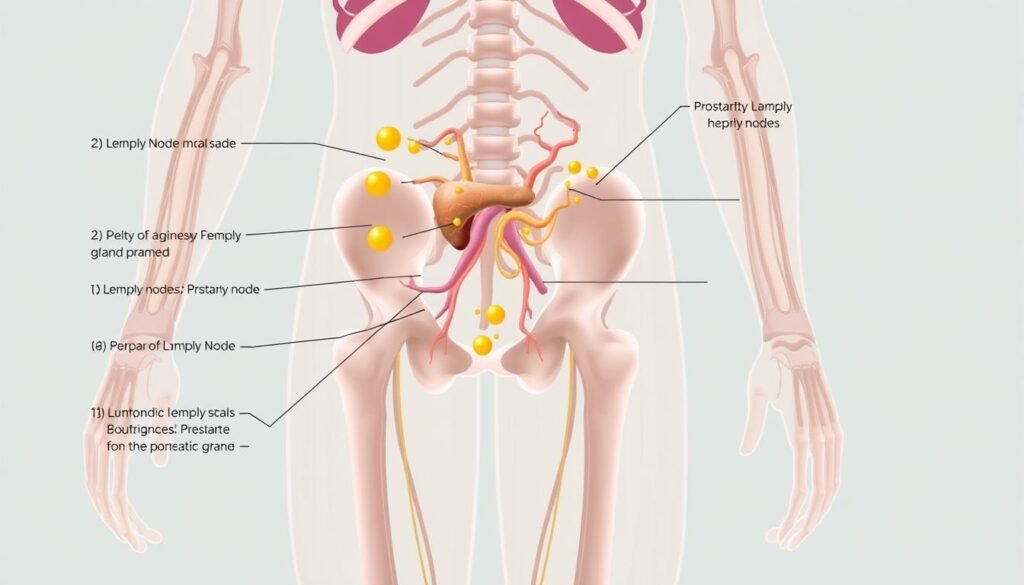
| Classification | Definition | Survival Rate |
|---|---|---|
| N0 | No lymph node involvement | Varies widely |
| N1 | Presence of cancer in nearby lymph nodes | 75-80% (1 LN), 20-30% (more than 5 LNs) |
Metastasis (M) in Prostate Cancer
Understanding how prostate cancer spreads is key in handling the disease. The “M” stage shows if the cancer moved past the prostate. It’s very important to know this for choosing the right treatment plan. This helps in dealing with the possible spread of cancer spread implications.
Understanding M0 and M1
M0 and M1 tell us if the cancer has spread. M0 means no spread. M1 means the cancer has spread. The M1 category is divided into parts:
- M1a: Cancer has reached lymph nodes outside the pelvis.
- M1b: There are bone metastases, showing the disease has advanced.
- M1c: Cancer has spread to other organs, showing widespread disease.
The Implications of Metastatic Spread
Metastatic spread changes treatment plans. People with M1 need more intense treatment. This might include chemotherapy or hormone therapy. These methods are different from early cancer treatment.
Knowing these categories helps doctors create better treatment plans. If you have prostate cancer, it’s important to understand how staging impacts treatment. Catching symptoms of metastasis early is also key. For more details, see the symptoms of stage 4 prostate cancer.
The Gleason Score: A Key Component in Staging
The Gleason score is very important when it comes to staging prostate cancer. It helps measure how aggressive the cancer is. Created in the 1960s, this system looks at cancer cells under a microscope. It gives grades from 1 to 5, based on what the biopsy samples show.
Generally, scores vary from 6 to 10, showing common grading for prostate cancer. When looking at biopsy samples, pathologists give two grades. The first grade is for the most seen tumor pattern, and the second is for the next most common. This forms a Gleason score, telling us how aggressive the cancer is. Cancers with a score of 6 are low grade. Meanwhile, scores from 7 to 10 indicate more serious cancers.
In 2014, a new system called the Grade Group was started. It made classification easier, putting cancers into five grades. This helps doctors create better treatment plans. Knowing the Gleason score helps figure out the patient’s risk level. It uses the cancer grade, PSA levels, tumor stage, and biopsy results. This full view supports making choices about treatment. With prostate cancer impacting over 1.6 million men every year, using the Gleason score with the TNM classification is key in helping patients.